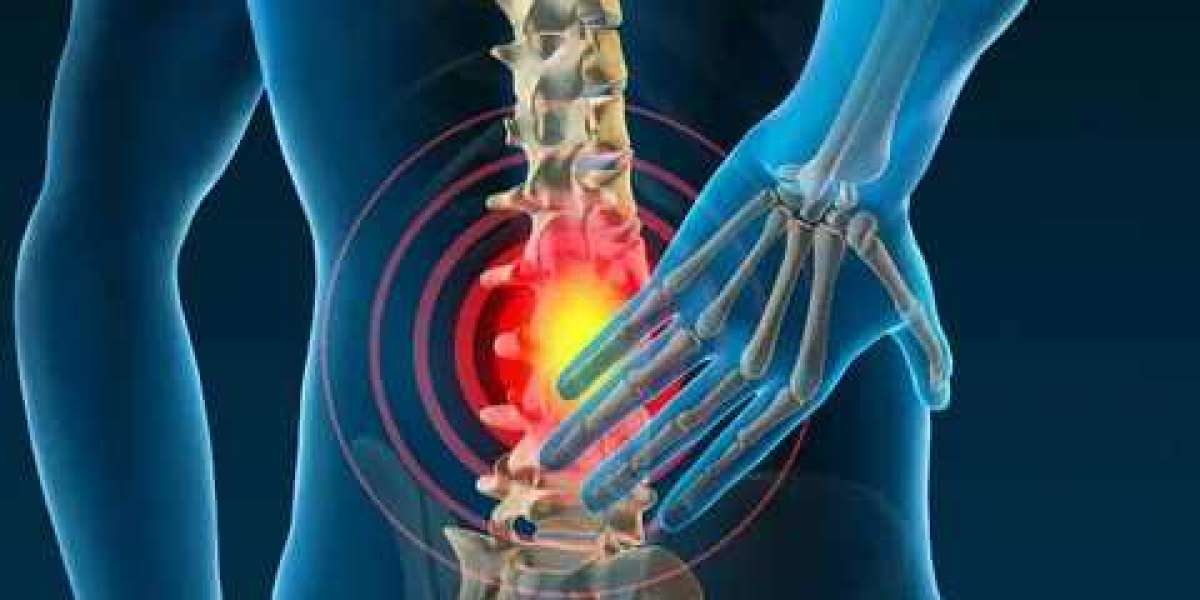
Research on the complex and developing genetic foundation of pain sensitivity has great potential to advance individualized medicine and pain management. Individual differences exist in how sensitive they are to pain, and heredity is a major factor in determining how sensitive a person is to pain, how well they respond to painkillers, and how likely they are to acquire chronic pain disorders. Through deciphering the genetic code responsible for pain sensitivity, scientists hope to find genetic risk factors, biomarkers, and possible targets for cutting-edge pain treatments. This article will discuss the impact of genetics on pain sensitivity, current developments in genetic research, and the implications for customized medicine and pain management.
I. Overview of Sensitivity to Pain
A. What Constitutes Pain Sensitivity
An individual's perception and reaction to pain stimuli are referred to as their pain sensitivity. It includes the point at which pain is felt, the degree to which pain is felt, and how long pain feelings last. Individual differences in pain sensitivity are common and are impacted by genetic, environmental, and psychosocial variables.
B. The Value of Sensitivity to Pain
Comprehending the sensitivity to pain is essential for efficient pain treatment and customized medication. Differences in pain sensitivity affect how well a person responds to painkillers, how effective pain therapies are, and how likely they are to acquire chronic pain disorders. In order to develop more specialized and successful pain management techniques, researchers want to uncover biomarkers and genetic targets by analyzing the genetic foundation of pain sensitivity.
II. Pain Sensitivity Genetics
A. Genetic Variants Linked to Sensitivity to Pain
Single Nucleotide Polymorphisms (SNPs): SNPs are common genetic variants that arise when an individual's single nucleotide base differs from another. Numerous single nucleotide polymorphisms (SNPs) have been found in genes associated with pain perception, including those that encode ion channels, neurotransmitters, and pain signaling receptors.
Genetic Risk Factors: A higher chance of having chronic pain problems or heightened sensitivity to pain have been linked to specific genetic variants. For instance, changes in pain sensitivity and response to opioid drugs have been linked to variances in the genes encoding for the catechol-O-methyltransferase enzyme (COMT) and the mu-opioid receptor (OPRM1).
B. Patterns of Pain Sensitivity Inheritance
Complicated Inheritance: There are several genetic and environmental factors that determine pain sensitivity, making it a complex trait. Instead of adhering to straightforward Mendelian inheritance patterns, it is characterized by the interaction of several genes, each of which influences the final phenotype.
Gene-Environment Interactions: An individual's pain response may be modulated by genetic variations linked to pain sensitivity interacting with environmental factors, like stress, trauma, or lifestyle choices. Deciphering the intricate genetic foundation of pain sensitivity requires an understanding of these gene-environment interactions.
III. Current Developments in Genetics
A. Studies of Genome-Wide Associations (GWAS)
Large-Scale Research:
Thousands of genetic variants have been linked to a variety of traits and disorders, including pain sensitivity, by genome-wide association studies (GWAS).
Pain Phenotypes:
GWAS research have shown genetic variations linked to particular pain phenotypes, including musculoskeletal pain, neuropathic pain, and migraine. These findings shed light on the genetic foundation of various forms of pain sensitivity.
B. Pain Sensitivity and Epigenetics
Gene control:
Epigenetic processes that affect pain sensitivity include DNA methylation, histone changes, and non-coding RNA control. These processes are critical to the expression of genes.
Environmental Factors:
An individual's pain sensitivity can be influenced by environmental factors that control epigenetic alterations, including stress, food, and exposure to chemicals.
IV. Consequences for Personalized Medicine and Pain Management
A. Pain medication pharmacogenetics
Tailored Care:
Pharmacogenetic analysis can assist in detecting genetic variations that affect a person's reaction to painkillers, including opioids, NSAIDs, and antidepressants.
Optimizing Treatment:
Healthcare professionals can maximize treatment efficacy, reduce side effects, and enhance patient outcomes by customizing painkillers based on a patient's genetic profile.
B. Personalized Treatments for Prolonged Pain
Precision medicine
Knowledge of the genetic underpinnings of chronic pain disorders can guide the creation of focused treatments that target certain pain pathways and processes.
Novel Drug Targets:
Ion channels, neurotransmitter receptors, and inflammatory mediators are a few examples of possible drug targets for novel pain therapeutics that have been found through genetic studies on pain sensitivity.
C. Biomarkers of Sensitivity to Pain
Predictive Biomarkers:
A person's propensity to acquire chronic pain disorders or how they will react to pain management therapies can be predicted by genetic biomarkers linked to pain sensitivity.
Early Intervention:
By enabling early intervention and customized treatment plans, the early discovery of genetic biomarkers for pain sensitivity can enhance patient outcomes and quality of life.
V. Difficulties and Prospects
A. Moral Points to Remember
Privacy and permission:
The possibility of genetic discrimination, patient privacy, and permission are among the ethical issues raised by genetic testing for pain sensitivity.
Stigma and Bias:
Genetic testing for pain sensitivity may be linked to stigma and bias, which makes patients and healthcare professionals reluctant to adopt customized medicine techniques.
B. Research on Translation
Bridging the Gap:
To develop and evaluate personalized medicine approaches for pain management, basic science researchers, clinicians, and industry partners must work together to translate genetic discoveries into clinical practice.
Implementation Challenges:
Cost, accessibility, and healthcare infrastructure may be issues for implementing genetic testing and customized medicine techniques for pain management.
VI. Concluding Remarks
In summary, the field of study on the influence of genetics on pain sensitivity is intricate and dynamic, with noteworthy consequences for the treatment of pain and customized medicine. Genetic variations affect a person's sensitivity to pain, how well they respond to painkillers, and how likely it is that they will acquire chronic pain disorders. Recent developments in genetics have revealed possible targets for innovative pain treatments and shed light on the genetic basis of pain sensitivity. Examples of these studies include genome-wide association studies and epigenetic studies. Comprehending the genetic code responsible for pain sensitivity has the potential to enhance personalized medicine methods, optimize therapy efficacy, and improve pain management for those with chronic pain problems. To fully realize the promise of genetic research in pain management, however, would need tackling the ethical, translational, and practical issues surrounding genetic testing and tailored medication.